Periodontosis: characteristics of the condition, causes, symptoms,
and modern treatment approaches
Periodontosis is one of the rarest yet most complex periodontal diseases, characterized by a slow and systemic destruction of periodontal tissues without a pronounced inflammatory component. Unlike periodontitis, where inflammation of the gums and the formation of periodontal pockets are the key mechanisms, periodontosis is defined by progressive tissue dystrophy and thinning, reduced blood supply, and impaired trophic support, which leads to atrophy of the bone structure and weakening of tooth stability. The disease develops gradually, often over many years, without pain or noticeable symptoms, making it particularly dangerous: patients usually seek help only when structural changes have already become irreversible.
Modern epidemiological reviews, including data from the European Federation of Periodontology (EFP, 2023), indicate that true periodontosis occurs in less than 2–5% of the population, while inflammatory periodontal diseases (gingivitis and periodontitis) affect more than 50–70% of adults. In the countries of the CIS, statistics are similar: according to the Russian Periodontology Society (2022), true periodontosis is diagnosed in approximately 3% of patients who visit a dentist. This explains the frequent cases of diagnostic confusion, where periodontitis is mistakenly called periodontosis. Understanding the difference between these conditions is crucial, since treatment strategies differ fundamentally.
Causes of Periodontosis
The etiology of periodontosis remains multifactorial and not yet fully understood. The most likely mechanism is hereditary predisposition associated with microcirculation characteristics and bone metabolism. Studies published in the Journal of Periodontal Research (2021) identify genetic markers that influence the activity of osteoblasts and osteoclasts, leading to reduced bone formation and accelerated resorption. Vascular disorders also play a significant role: when the blood supply to the periodontal tissues decreases, the gums receive less oxygen and nutrients, and bone tissue becomes more fragile.
Associated contributing factors may include endocrine disorders (especially diabetes mellitus and hypothyroidism), vitamin D and calcium deficiency, neurotrophic dysfunctions, and long-term chronic systemic diseases. However, the key difference between periodontosis and periodontitis is the absence of active inflammation. This is precisely why patients often fail to notice symptoms until the disease has progressed significantly.
Symptoms and Characteristic Manifestations
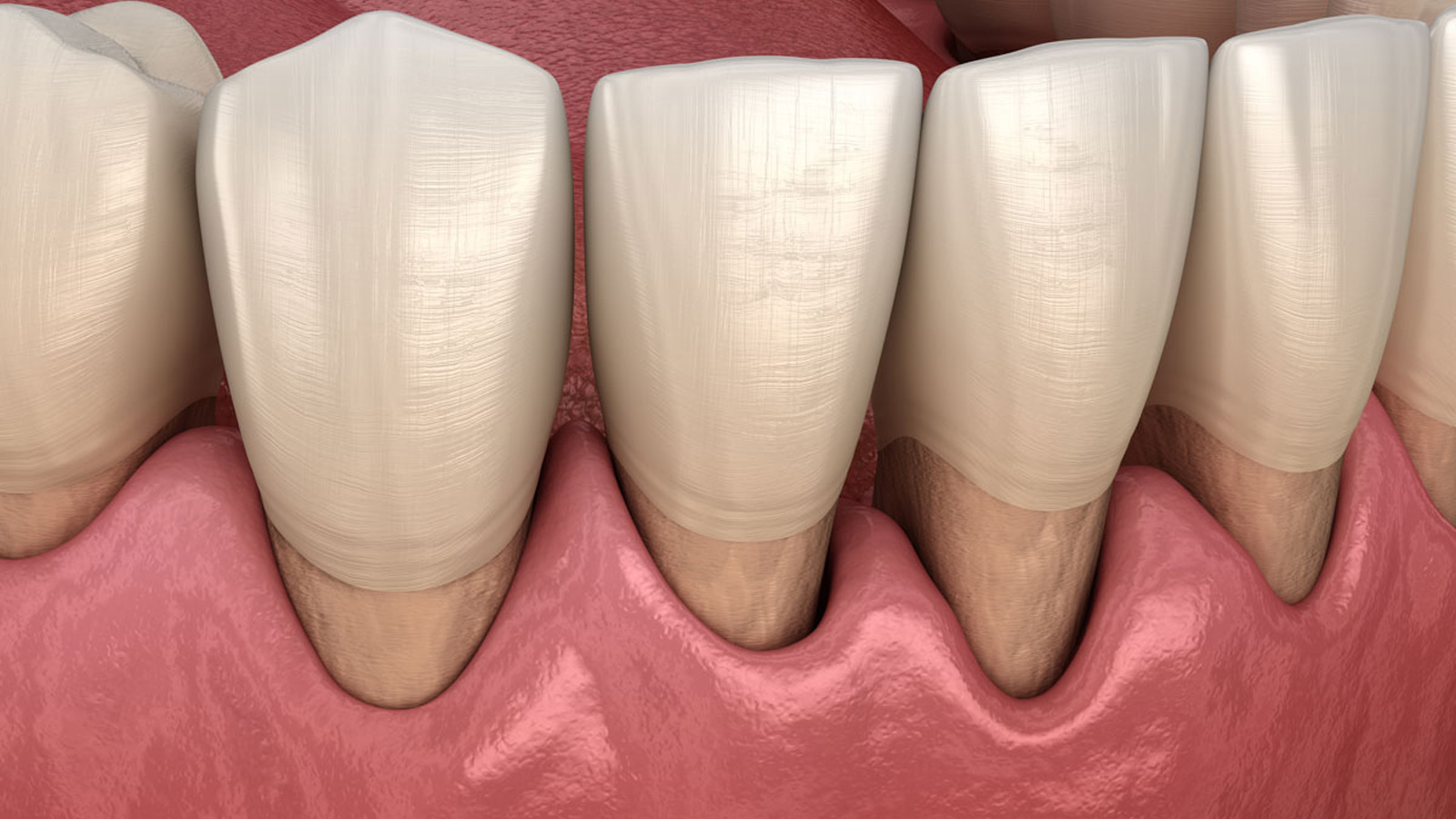
In its early stages, periodontosis causes almost no pain or discomfort. Gradually, patients may notice a sensation of “exposed teeth” and increased sensitivity to hot and cold. The enamel may appear more translucent, and the crowns of the teeth may appear visually longer due to the slow recession of the gums. As the condition progresses, alveolar bone atrophy develops, teeth begin to loosen, the bite may change, and the dental arch may feel weakened.
Periodontosis is not associated with bleeding, pronounced redness, or swelling of the gums — such signs are typical of periodontitis. Radiographic examination reveals uniform bone resorption without the formation of deep periodontal pockets, which is the main differential diagnostic indicator.

Why Early Treatment Is Essential
Periodontosis leads to the loss of structural support of the teeth and may result in tooth loss even in the absence of symptoms. Bone tissue that has lost density and volume does not regenerate on its own. The earlier treatment begins, the greater the chance of stabilizing the condition and slowing the atrophic processes.
Timely diagnosis includes panoramic X-ray imaging, CT scans of the jaws, evaluation of periodontal attachment levels, and consultation with a periodontist. At Diplomat Med Center, diagnostics are performed using advanced digital technologies, allowing pathological changes to be detected at early stages and enabling personalized treatment planning.
Modern Treatment Methods for Periodontosis
Treatment focuses on improving blood circulation, stimulating regeneration of bone tissue, and strengthening the ligamentous apparatus of the teeth. Regenerative technologies are utilized, including osteoplastic materials, barrier membranes, platelet-rich fibrin and plasma (PRF/PRP) therapies, and stem cell–based treatments. These methods activate natural reparative processes and increase bone density in areas affected by atrophy.
Physiotherapeutic and microcirculatory techniques (laser therapy, deep photobiostimulation, ozone protocols) improve tissue metabolism. Additionally, remineralization therapy is recommended to strengthen enamel and reduce sensitivity. Proper oral hygiene plays a crucial role: selecting the correct toothbrush, toothpaste, and irrigator, and mastering proper brushing techniques.
Treatment of Periodontosis at Diplomat Med Center
At Diplomat Med Center, treatment is comprehensive, taking into account microcirculation, dental aesthetics, and bone condition. During the diagnostic stage, we perform digital scanning, radiography, or CT imaging to determine the degree of atrophy and develop a personalized treatment plan. If necessary, oral sanitation is performed, including treatment of caries, restoration of gum health, and orthodontic correction.
We use membrane technologies, bone graft substitutes, and regenerative therapy aimed at improving bone density and stabilizing the dental arch. This approach allows for significant slowing of disease progression and preservation of the teeth for many years.
Schedule a consultation — we will select a treatment program that corresponds to the stage of periodontosis and your individual anatomical features.
Diplomat Med Center — caring for your smile and your health for years to come.